Validation of a Predictive Model of Vaginal Birth after Caesarean Section in Pakistani Women
By Asra Bari, Riffat Jaleel, Shehla ArifAffiliations
doi: 10.29271/jcpsp.2024.04.440ABSTRACT
Objective: To determine the frequency of successful trials of vaginal birth after Caesarean section (VBAC) using the Flamm and Geiger model.
Study Design: Observational study.
Place and Duration of the Study: Obstetrics and Gynaecology Unit II of Dr. Ruth K.M. Pfau Civil Hospital, Karachi, Pakistan, from August 2022 to January 2023.
Methodology: Women with singleton pregnancy having cephalic presentation, previous one lower segment caesarean section (LSCS), and without any contraindication for vaginal delivery were included. Women bearing foetus having estimated weight >3.5kg, morbid obesity, multiple pregnancies, non-cephalic presentation, placenta praevia, abruptio placentae, uncontrolled maternal comorbidities, or had previous two or more Caesarean sections were excluded. Flamm and Geiger score was applied to record observations of successful and unsuccessful trials. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the score were calculated by ROC curve, along with its area under the curve (AUC) and Youden’s index curve, with 95% confidence interval.
Results: This study included 258 participants. Successful vaginal delivery was possible in 125 (48.4%) participants, whereas 133 (51.6%) underwent emergency Caesarean section. Cervical dilatation and effacement were the main factors assessing the success. The Flamm and Geiger score of >5 had an area under the curve of 0.813 (0.762-0.864). The score's sensitivity was 75% (67-82%), specificity 76% (68-82%), and PPV of 75% with an accuracy of 76%.
Conclusion: The Flamm and Geiger score of >5 demonstrated high sensitivity, specificity, PPV, and accuracy in predicting later successful vaginal birth. It is recommended as a promising and valuable tool for assessing VBAC's success in low-resource countries.
Key Words: Vaginal birth after caesarean, Flamm and Geiger Model, Indication of caesarean, trial of labour after caesarean, VBAC risk scoring criteria.
INTRODUCTION
Globally caesarean section (CS) rates have increased from approximately 7% in 1990 to 21% in 2022.1 According to the latest Pakistan demographic and health survey, the CS rate has increased over the past few years from 14% in 2012-13 to 22% in 2017-182 lagging far behind the WHO recommendation of 10%.3 A careful trial of labour after caesarean (TOLAC) may reduce the number in approximately 75% of cases.4
Although labour is a painful experience, TOLAC is generally safe both for the mother and foetus in most cases.5 It also reduces morbidity related to elective repeat Caesarean section (ERCS), such as shorter hospital stays, reduced blood loss, less infection, thromboembolic events, need for transfusion, and foetal hypoxia.5 Failed TOLAC resulting in emergency CS has its own fetomaternal morbidity and it also causes psychological distress to the mother.6 Therefore, to overcome this problem, a standardised scale should be employed to categorise patients who would benefit from a trial of scar.7
Among the various available tools, Flamm and Geiger is a well-known and established scoring criterion offering reasonable predictability for trial of scar in high risk women.8 It considers woman's age, cervical dilatation and effacement on admission, prior vaginal birth and indication of previous CS. All findings are given points ranging from 0 - 4 and a score of >4 is associated with high success rates. Reaching term pregnancy with prior CS is made challenging by a number of risk factors in terms of choosing the induction method and timing. It is important to remember that these models and scoring systems are not definitive and cannot guarantee successful outcomes but can only indicate a likelihood.6,9 Healthcare providers should make a careful decision in consultation with pregnant individuals considering their circumstances, preferences, and other medical conditions.3,4,7,10
A number of researches have been conducted throughout the world but the data on Pakistani population is still lacking due to differences in genetics and socioeconomic dynamics, so this research was conducted to test the scoring system and find out the frequency of successful TOLAC as predicted by Flamm and Geiger model.
METHODOLOGY
This observational study was conducted from 1st August 2022 to 31st January 2023 in the Obstetrics and Gynaecology Unit II of Dr. Ruth K.M. Pfau Civil Hospital, Karachi. Approval from the institutional review board (IRB) was taken. Sample size was calculated by area under the curve (AUC) for the Flamm and Geiger model which was determined to be 0.777 (95% CI 0.69, 0.85, p <0.0001), sensitivity and specificity at 72% and 76%, respectively, with a cut-off score of 5. To maintain a 5% desired precision level within a 95% confidence interval, a total of 258 women were enrolled in the study. Women aged between 18 to 45 years were recruited meeting inclusion and exclusion criteria and delivering at the study unit. Women having singleton pregnancy with vertex presentation, previous one LSCS, gestational age of 32 to 41 weeks, and no contraindication to vaginal delivery were included. Women with estimated foetal weight >3.5 kg, morbid obesity, multiple pregnancies, non-cephalic presentation, placenta previa, abruptio placen-tae, uncontrolled diabetes and hypertension, previous two or more CS, history of uterine rupture, previous classical CS, and who refused to participate were excluded. Written and informed consent was taken at the time of admission.
After admission to labour ward, detailed history and examination were conducted. Data were collected via proforma that was filled in by the researcher. It included demographic characteristics, past obstetric history, inter-delivery interval, indication of previous CS, ante- and postpartum course, pre-existing medical conditions, and characteristics of present pregnancy (gestational diabetes, preeclampsia, rupture of membranes and placental localisation etc.). Obstetric abdominal examination was performed to assess foetal weight, lie, presentation, amount of liquor, engagement, and uterine contractions. Vaginal examination included cervical dilation and effacement, presence of membranes, and colour of liquor. Labour was diagnosed as regular and painful uterine contractions causing progressive dilatation and effacement of the cervix.
Trial of labour was offered after full counselling of pros and cons. Flamm and Geiger score was applied to assess favourability for TOLAC. No pharmacological method was implied either for induction or augmentation of labour. Women having spontaneous onset of labour were admitted right away and non-labouring women were induced via intracervical foleys. Parturients were monitored via vital signs and, abdominal and vaginal examination. Foetal monitoring was done via cardiotocograph (CTG) and intermittent auscultation. The labour care guide was used to monitor the events of labour. Scar dehiscence was suspected in cases of maternal tachycardia, presence of scar tenderness, foetal bradycardia, loss of beat-to-beat variability, and vaginal bleeding. The trial of scar was abandoned if any suspicion of foetal hypoxia, non-progress of labour or impending scar dehiscence was observed. Active management of the third stage of labour was done as recommended by WHO. Fetomaternal complications following delivery were noted. The patients were divided into two groups; one comprising those with successful VBAC and the other with failed TOLAC, and their characteristics were compared.
Data were analysed using SPSS-22 (IBM, IL, USA) and Python 3.8.14 using mean, range, and SD values as appropriate for continuous variables and frequencies with percentages for categorical variables. The proportions were compared using the c2 test. The mean difference between successful vs. failed TOLAC was applied using an independent sample t-test. The prospective validity of the Flamm and Geiger model was determined by plotting the ROC curve and its AUC with a 95% confidence interval (CI). The major discriminating point of the Flamm and Geiger score was established by computing Youden’s J statistic and the sensitivity, specificity, PPV, and NPV with 95% CI of the score at different discriminating points. A p ≤0.05 was considered statistically significant in all analyses.
RESULTS
Two hundred and fifty-eight participants were enrolled in this study with mean age was 27 ± 5 (18 - 44) years. Half of the participates were of age 26-35 years 129 (50%). One hundred and fifty (58.1%) participants were second parous (gravida 1), one third (79, 30.6%) para 3 - 4, and others (29, 11.2%) were 5 and above. The participants belonged to a range of ethnicities, including 79 Muhajir (30.6%), 73 Pathan (28.3%), 37 Sindhi (14.3%), 25 Punjabi (9.7%), and 21 others (8.1%). The mean BMI was 27.1 ± 5.2 (15.59 - 54.88) kg/m2, and the majority 199 (77.1%) were overweight. About half 132 (51.2%) of babies’ birth weight belonged to 2.6 to 3.0 kg. More than half 162 (62.8%) were term and the rest were preterm. It was found that 51 (19.8%) participants had history of vaginal birth before CS, 38 (14.7%) delivered after, and 19 (7.4%) experienced vaginal birth both before and after CS. All women belonged to the poor socioeconomic class. Table I shows the association between cervical dilatation and effacement to successful VBAC. A total of 125 (48.4%) patients had successful vaginal delivery, whereas 133 (51.6%) ended up in emergency Caesarean section.
Table I: Outcome of VBAC with cervical effacement and dilatation.
|
- |
Successful VBAC n (%) |
Failed TOLAC n (%) |
Total n (%) |
p-value |
|
- |
125 (48.4) |
133 (51.6) |
258 (100) |
- |
|
Cervical effacement (%) |
- |
- |
- |
- |
|
>75% |
24 (19.2) |
1 (0.8) |
25 (9.7) |
- |
|
25 - 75% |
96 (76.8) |
88 (66.2) |
184 (71.3) |
<0.001* |
|
<25% |
5 (4) |
44 (33.1) |
49 (19) |
- |
|
Cervical dilatation (cm) |
- |
- |
- |
- |
|
≤4 cm |
47 (37.6) |
125 (94) |
172 (66.7) |
- |
|
>4 cm |
78 (62.4) |
8 (6) |
86 (33.3) |
<0.001* |
|
VBAC: Vaginal birth after Caesarean; TOLAC: Trial of scar after Caesarean. |
||||
Table II: Distribution of Flamm and Geiger score to success rates of VBAC.
|
Flamm Score |
Successful VBAC n (%) |
Failed TOLAC n (%) |
Total n |
|
2 |
1 (14.3) |
6 (85.7) |
7 |
|
3 |
5 (11.4) |
39 (88.6) |
44 |
|
4 |
25 (30.9) |
56 (69.1) |
81 |
|
5 |
27 (57.4) |
20 (42.6) |
47 |
|
6 |
29 (80.6) |
7 (19.4) |
36 |
|
7 |
19 (90.5) |
2 (9.5) |
21 |
|
8 |
12 (85.7) |
2 (14.3) |
14 |
|
9 |
5 (83.3) |
1 (16.7) |
6 |
|
10 |
2 (100) |
0 (0) |
2 |
|
VBAC: Vaginal birth after Caesarean. |
|||
Table III: The association of successful vs. failed TOLAC with different demographic and clinical parameters.
|
Demographics and clinical |
Successful |
Failed TOLAC |
Total |
p-value |
|
Age (years) |
27.4 (±5.2) |
27.4 (±5) |
27.4 (±5.1) |
0.943 |
|
Parity |
2.1 (±1.3) |
1.7 (±1.4) |
1.9 (±1.4) |
<0.001* |
|
BMI (Kg/m2) |
27.1 (±5.4) |
27.1 (±5) |
27.1 (±5.2) |
0.977 |
|
Baby weight (Kg) |
2.8 (±0.4) |
2.8 (±0.4) |
2.8 (±0.4) |
0.204 |
|
Gestation age (weeks) |
37.8 (±1.9) |
37.7 (±1.8) |
37.7 (±1.8) |
0.422 |
|
Cervical effacement (%) |
58.6 (±21.8) |
30.8 (±14.9) |
44.2 (±23.2) |
<0.001* |
|
Cervical dilatation (cm) |
5.4 (±2.2) |
2.8 (±1.2) |
4.1 (±2.2) |
<0.001* |
|
Interpregnancy Interval (IPI) in months |
49.1 (±32.4) |
39.5 (±27.4) |
44.2 (±30.2) |
<0.001* |
|
Flamm score |
5.8 (±1.6) |
4 (±1.2) |
4.9 (±1.7) |
<0.001* |
|
VBAC: Vaginal birth after Caesarean; TOLAC: Trial of scar after Caesarean. |
||||
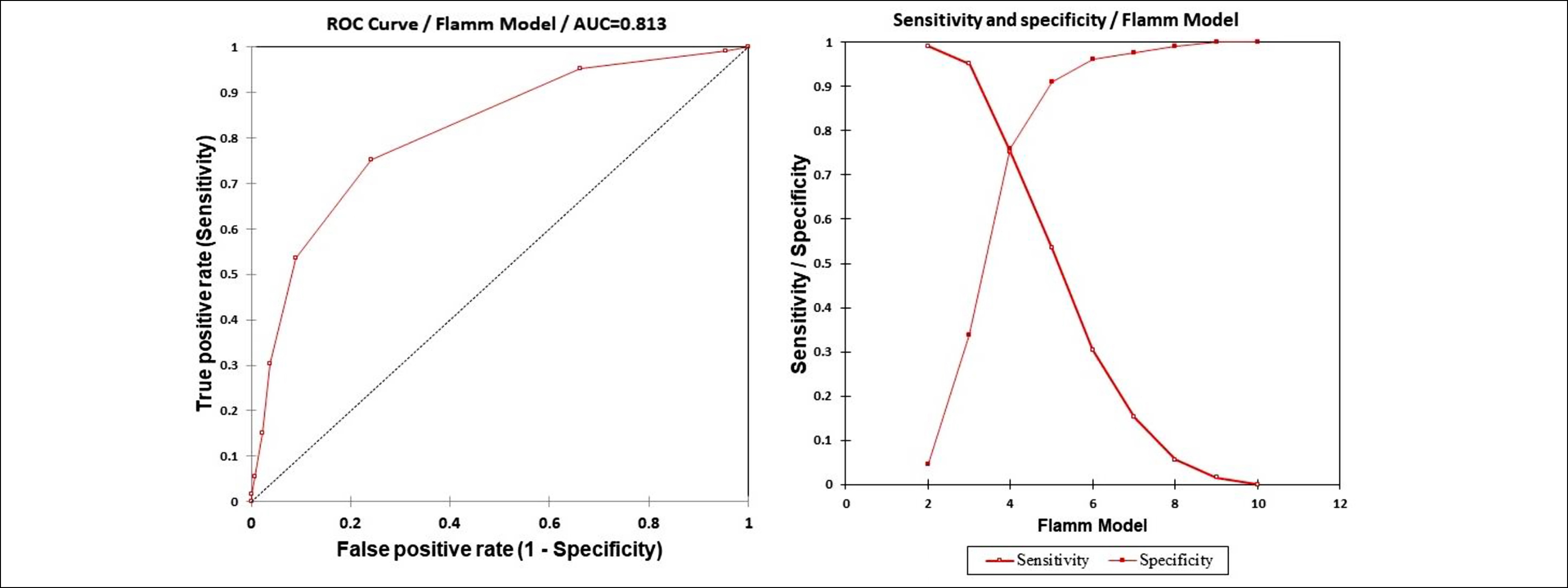 Figure 1: Receiver operator curve for the Flamm characteristics scoring system for successful VBAC exhibiting area under the curve (AUC) and Youden index curve best cut-off (sensitivity + specificity) index curve.
Figure 1: Receiver operator curve for the Flamm characteristics scoring system for successful VBAC exhibiting area under the curve (AUC) and Youden index curve best cut-off (sensitivity + specificity) index curve.
The trial of scar was abandoned in 133 (51.6%) patients due to signs and symptoms of impending uterine rupture 62 (46.6%), non-progress of labour 24 (18%), failed induction 12 (9%), ruptured uterus 6 (4.5%), and foetal distress 29 (21.85%). Table II shows the relationship of different scores to the chances of successful VBAC. A higher Flamm and Geiger score is related to better chances of successful VBAC. The success rates were more than 80% when the score was ≥6.
Non-progress of labour as a cause of previous caesarean section was observed in 29 (11.2%) and the rest had other indications. Pre-existing diabetes was present in 14 (5.4%) and hypertension in 23 (8.9%). GDM with obstetric cholestasis documented in 2 (0.8%) and 11 (4.3%) had hypertensive disorders of pregnancy. Few (7, 2.7%) had ruptured membranes at the time of admission. Table III demonstrated the correlation of both groups i.e. successful and failed TOLAC with different parameters. Cervical efface-ment, dilatation, interpregnancy interval (IPI), and increasing Flamm and Geiger scores were significantly associated to a success-ful trial of scar p <0.001.
Figure 1 shows that Flamm and Geiger scores of >5 had an area under the curve of 0.813 (0.762 - 0.864). The score's sensitivity was 75% (67% - 82%), specificity 76% (68% - 82%), and positive predictive value of 75% with an accuracy of 76%. None of the patients experienced post-delivery scar rupture and there was no case of maternal death was reported.
DISCUSSION
This study showed that advanced cervical dilatation and effacement are strong predictors for successful TOLAC in the Flamm and Geiger model. Apart from this, multiparity and interpregnancy interval were also found to favour successful TOLAC. The findings of this study revealed an insignificant relationship in women with and without a history of previous vaginal birth after caesarean unlike other studies. Failure of the trial was a result of signs and symptoms of impending rupture, prolonged labour, foetal distress, and failed induction while most patients with scores of ≥5 had successful VBAC, many patients with a total score of ≤3 at the time of admission underwent an EmCS. Overall, with an advance total score the likelihood of a successful VBAC also increased which is comparable to other studies.11,12 Age and ethnicity did not offer statistically significant differences between the two groups under consideration.
Of the 258 patients who underwent TOLAC, 52.6% undergone EmCS which is equivalent to study by Panchal et al.13 This high C/S rate is due to a greater number of referrals, lack of antenatal care, unbooked patients, and iterative caesareans in the hospital. The current study confirmed the findings of Ray et al.11 that scar tenderness was the most frequent cause of EmCS in patients undergoing TOLAC. A similar incidence of the most feared complication of TOLAC i.e. uterine rupture was also found by Takeya et al. in Japan.14
Several studies report a higher success rate of VBAC which differs from the findings of this study15-18 owing to factors, such as better antenatal care, less infection, strong scars, good nutrition, and efficient intrapartum care. Various studies from different regions report a success rate compar-able to this study.19,20 Overall low success rates were observed from India,21 South Africa,22 Australia.23 It is postulated that low-resource settings cannot provide vigilant care for TOLAC efficiently which includes one-to-one care, continuous electro-nic foetal monitoring, and availability of operating rooms.
Strengths of the study include high patient turnover at the place belonging to a wide range of ethnicities from all over the country. This eliminated any influence on results owing to differences in genetics.
Limitations of this study included difficulty in assessment of scar strength which cannot be measured reliably by any means and usually is not good presumably related to a high rate of post-partum infections and poor nutritional status of Pakistani women. Other contributory factors were non- availability of continuous CTG or foetal blood sampling, over burdening of labour staff, unbooked patients, and increased referrals, therefore a low threshold for CS was kept. There was a high rate of uterine rupture in contrast to one reported in the literature because of the same reasons.20 This necessitates the application of a validated score like Flamm and Geiger to reduce fetomaternal morbidity and burden on the healthcare system and facilitate clinicians and patients alike. Another similar model i.e. Grobman’s with some alterations was used by Wen et al.24 Although their success rate for VBAC was higher, the model had AUC comparable to the score used in this study, reinforcing the fact that scoring systems provide great help in decision-making.
CONCLUSION
This study depicted a high accuracy for the prediction of success of the trial of scar while using the Flamm and Geiger scoring system. Clinicians should take advantage of such validated scoring systems to counsel patients and make informed decisions regarding their mode of delivery.
ETHICAL APPROVAL:
Ethical approval was obtained from the institutional review board prior to the initiation of study.
COMPETING INTEREST:
The authors declared no conflict of interest.
PATIENTS’ CONSENT:
informed consent was obtained from the patients to publish the data.
AUTHORS’ CONTRIBUTION:
AB: Conceived, designed and wrote the content, and is responsible for the integrity of the research, data collection and literature search.
SA: Reviewed and corrected manuscript and interpreted results.
RJ: Review and final approval of the manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of Caesarean section rates: global and regional estimates. BMJ Glob Health 2021; 6(6):e005671. doi: 10.1136/bmjgh-2021-005671.
- Patel KK, Rai R, Rai AK. Determinants of infant mortality in Pakistan: Evidence from Pakistan demographic and health survey 2017-18. J Public Health (Berl.) 2021; 29:693-701 (2021). doi:10.1007/s10389-019-01175-0
- Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM. WHO working group on caesarean section. WHO statement on caesarean section rates. BJOG 2016; 123(5):667-70. doi: 10.1111/1471-0528.13526.
- Denison FC, Aedla NR, Keag O, Hor K, Reynolds RM, Milne A, et al. Royal college of obstetricians and gynaecologists. Care of women with obesity in pregnancy: Green-top guideline No. 72. BJOG 2019; 126(3):e62-106. doi: 10.1111/ 1471-0528.15386.
- Abdulrahman NB, Ismail SK. Factors associated with success of vaginal birth after cesarean section in association to maternal and neonatal outcomes. Sch Int J Obstet Gynec 2021; 4(7):282-90. doi: 10.36348/sijog.2021.v04i07.001
- Metz TD, Stoddard GJ, Henry E, Jackson M, Holmgren C, Esplin S. Simple, validated vaginal birth after Cesarean delivery prediction model for use at the time of admission. Obstet Gynecol 2013; 122(3):571-8. doi: 10.1097/AOG. 0b013e31829f8ced.
- Patel MD, Maitra N, Patel PK, Sheth T, Vaishnav P. Predicting successful trial of labor after cesarean delivery: Evaluation of two scoring systems. J Obstet Gynaecol India 2018; 68(4):276-82. doi: 10.1007/s13224-017-1031-2.
- Flamm BL, Geiger AM. Vaginal birth after cesarean delivery: An admission scoring system. Obstet Gynecol 1997; 90(6):907-10. doi: 10.1016/s0029-7844(97)00531-0.
- Mekonnen BD, Asfaw AA. Predictors of successful vaginal birth after a cesarean section in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy and Childbirth 2023; 23(1):1-12. doi:10.1186/s12884-023-05396-w.
- Angolile CM, Max BL, Mushemba J, Mashauri HL. Global increased cesarean section rates and public health implications: A call to action. Health Sci Rep 2023; 6(5):e1274. doi: 10.1002/hsr2.1274.
- Ray P, Mondal A, Ray P. Outcome of vaginal birth after cesarean section: A prospective study. Int J Sci Stud 2016; 4(9):119-22. doi: 10.17354/ijss/2016/628.
- Tesfahun TD, Awoke AM, Kefale MM, Balcha WF, Nega AT, Gezahegn TW, et al. Factors associated with successful vaginal birth after one lower uterine transverse cesarean section delivery. Sci Rep 2023; 13(1):8871. doi: 10.1038/ s41598-023-36027-1.
- Panchal A, Soni A, Joshi P, Vaishnav G, Pagi S. Analytical study of factors determining success rate of trial of scar (TOS). Int J Med Sci Public Health 2015; 4(6):853-8. doi:10. 5455/ijmsph.2015.01022015178.
- Takeya A, Adachi E, Takahashi Y, Kondoh E, Mandai M, Nakayama T. Trial of labor after Cesarean delivery (TOLAC) in Japan: Rates and complications. Arch Gynecol Obstet 2020; 301(4):995-1001. doi: 10.1007/s00404-020-05492-8
- Shaheen N, Khalil S, Iftikhar P. Prediction of successful trial of labour in patients with a previous caesarean section. J Pak Med Assoc 2014; 64(5):542-5.
- Khan B, Deeba F, Bashir R, Khan W. Outcome of trial of scar in patients with previous caesarean section. J Ayub Med Coll Abbottabad 2016; 28(3):587-90.
- Hassan A. Trial of scar and vaginal birth after caesarean section. J Ayub Med Coll Abbottabad 2005; 17(1):57-61.
- Mi Y, Qu P, Guo N, Bai R, Gao J, Ma Z, et al. Evaluation of factors that predict the success rate of trial of labor after the cesarean section. BMC Pregnancy Childbirth 2021; 21(1):527. doi: 10.1186/s12884-021-04004-z.
- Girma Y, Menlkalew Z, Destaw A. Vaginal delivery after caesarean section and its associated factors in mizan tepi university teaching hospital, Southwest Ethiopia. Heliyon 2021; 7(11):e08276. doi: 10.1016/j.heliyon.2021.e08276.
- Siraneh Y, Assefa F, Tesfaye M. Feto-maternal outcome of vaginal birth after cesarean and associated factors among mothers with previous cesarean scar at attat lord merry primary hospital, gurage zone, South Ethiopia. J Preg Child Health 2018; 5(5):390. doi: 10.4172/2376- 127X.1000390.
- Sahu R, Chaudhary N, Sharma A. Prediction of successful vaginal birth after caesarean section based on flamm and geiger scoring system a prospective observational study. Int J Reprod Contraception Obstetr Gynecol 2018; 7(10): 3998-4003. doi:10.18203/2320-1770.ijrcog2018 4118.
- Rubgega FD, Soma-Pillay P, Becker P. Caesarean section indications and outcomes at a tertiary level hospital in South Africa. O & G Forum 2021; 31(3):8-11. doi: 10.10520/ ejc-medog_v31_n3_a3.
- Toohill J, Gamble J, Creedy DK. A critical review of vaginal birth rates after a primary caesarean in Queensland hospitals. Aust Health Rev 2013; 37(5):642-8. doi:10.1071/ AH13044.
- Wen J, Song X, Ding H, Shen X, Shen R, Hu L, et al. Prediction of vaginal birth after cesarean delivery in Chinese parturients. Sci Rep 2018; 8(1):3084. doi: 10.1038/s41598- 018-21488-6.